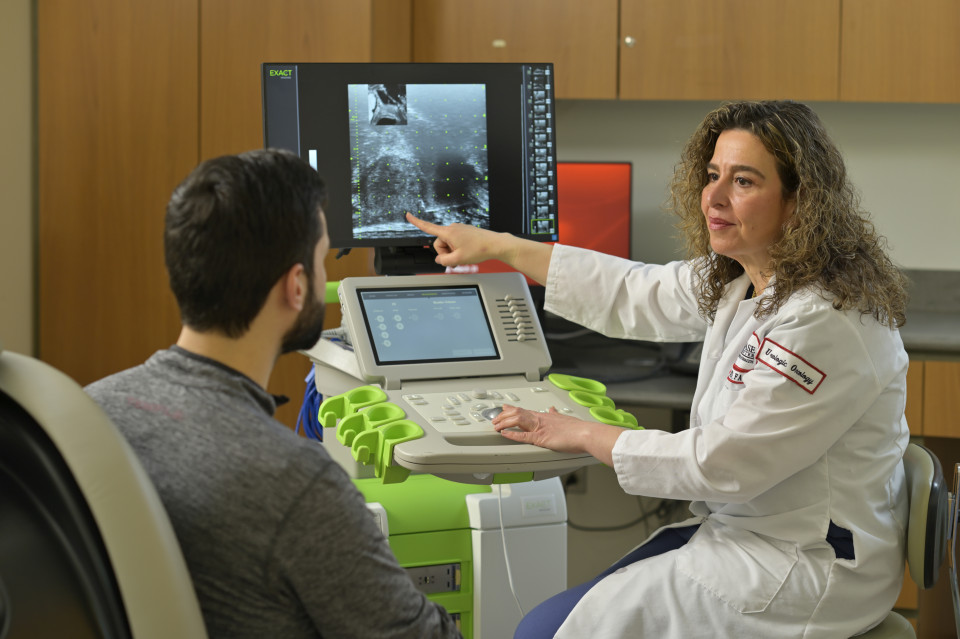
This New Ultrasound Technology at Fox Chase Could Help the Thousands of Men Living with Prostate Cancer
To many men and their loved ones, the prospect of prostate cancer is frightening. It’s the second most common cancer among men, and treatment can carry severe risks, including loss of sexual function and continence.
At the same time, prostate cancer is often treatable through surgery, radiation, and other means. And because of the slow-growing nature of some prostate cancers, patients may be able to put off treatment for some time or indefinitely without significant negative consequences, living fully despite the cancer or need for treatment.
How you monitor prostate cancer is therefore critical to patients’ quality of life, both before and after surgery or definitive treatment. Early detection and consistent surveillance can radically change outcomes. That’s why a new technology that allows physicians at Fox Chase Cancer Center to better see and analyze the cancer could revolutionize prostate cancer treatment—not only potentially saving lives, but changing the way we think about prostate cancer itself. Here’s how the new micro-ultrasound technology could transform prostate cancer treatment.
Current ultrasounds can make the first step in treatment difficult.
Typically, when a physician suspects a patient may be at risk of prostate cancer—usually after blood test results show an unusually high level of prostate-specific antigens (PSAs) or an abnormal digital rectal exam—they’ll perform a biopsy of the prostate guided by a standard ultrasound. The ultrasound allows for visualization but is not clear enough for the doctor to do much beyond taking a blind sample of the prostate.
“It’s usually random,” says Dr. Rosalia Viterbo, a urologic oncologist at Fox Chase Cancer Center. “It’s hard to tell if a suspicious lesion is present and can easily be missed.” In taking a simple random sample, it’s possible that a cancerous section of the prostate could remain undetected, so if your PSA level remains high after several months have passed, the physician may perform another biopsy.
Not only are repeated biopsies uncomfortable, they can carry risks. Infection, bleeding and scar tissue can result, and Viterbo has had some patients refuse to receive multiple biopsies after prior unpleasant experiences.
The alternative isn’t possible for everyone.
Viterbo describes MRIs as the “gold standard” for detecting even small cancerous lesions, and therefore the preferred option over ultrasounds. But MRIs are notoriously expensive.
“It has to be approved by insurance,” Viterbo says. “Half the time it is, and half the time it’s not.” According to Viterbo, a typical man as old as fifty, even with an elevated PSA, might not be approved.
Given the expense, it can’t be used routinely for regular detection, and the physician has to provide significant evidence of cancer risk or prior biopsy to obtain even one MRI. In any case, after that process, the physician still needs to perform a biopsy if a suspicious lesion is detected by MRI.
And some patients know they will never get an MRI. They may lack insurance, or be physically unable due to implants, hip replacements, obesity or claustrophobia. Even for people who can get an MRI, the extra hospital visit and the process as a whole can be stressful enough that it’s put off or refused. For patients in underserved communities, who are acting as caregiver, have special needs or don’t have access to transportation, it might not even be possible.
The micro-ultrasound enables regular, reliable detection.
The newly developed ExactVu Micro-Ultrasound System is as easy to perform as a standard ultrasound, right in the physician’s office, without any insurance process. But it provides visual clarity comparable to an MRI. For Viterbo, that means she can regularly detect, analyze and monitor suspicious lesions, and easily target the lesion with a biopsy without the need for MRI.
“It characterizes the architecture of cells,” Viterbo says. “I can monitor and assess, ‘Has it gotten bigger? Has it gotten more worrisome or aggressive? Is it trying to escape outside the prostate?’”
This makes early detection immediately more accessible. Even a family history of prostate cancer, without a PSA test, can justify a quick, often less-than-15-minute prostate exam as part of a larger appointment—with the added benefit of cutting down on hospital visits and insurance denials. That means accessibility is increased, which could help success rates overall.
“It does affect a patient’s ability to be screened, and not to miss something that could go from something treatable or confined with surgery or radiation, to something that spreads because of their reluctance to have another biopsy or MRI,” Viterbo says.
It also enables added reassurance for what oncologists call “active surveillance.” Low-risk prostate cancer can remain relatively stable for years, meaning that patients can forgo the risk of surgery or radiation for a significant period of their lives with regular monitoring. With the micro-ultrasound, instead of unpleasant, repeated biopsies that only produce random samples, these patients may simply require a micro-ultrasound exam to ease their worries.
It can help improve cancer treatment.
It’s not just detection—Viterbo points out that the new technology could aid her in reaching desired surgical outcomes.
For one, it allows her to get patients into the operating room at the right time. Where treatment may have been delayed due to the complex insurance process of obtaining an MRI, she can now catch and recognize potentially fast-growing cancers almost immediately and get those patients scheduled as quickly as possible.
She also has the ability to recognize cases where the patient has a less-aggressive cancer and would be better off with time to prepare for surgery, by getting vaccinated against COVID, for example, or getting to a healthy weight, and scheduling them accordingly.
While it’s still early, Viterbo thinks that the technology will also allow her to better plan for surgery. If time has passed between biopsy and surgery, she can do a re-examination to check if anything has changed. By knowing with greater clarity the borders of the cancerous area and the degree of aggressiveness of the cancer, she can pursue wide margins and help ensure all cancer is completely removed. On the other hand, she also hopes to improve recovery for sexual function and continence thanks to that granularity, since it helps her to navigate around critical areas with less risk.
“Otherwise, it’s just kind of a blind perspective if I can’t get an MRI,” Viterbo says. “This way I feel confident I’m not missing potentially dangerous cancer.”
Learn more about how Fox Chase Cancer Center is at the forefront of cancer care.
This is a paid partnership between Fox Chase Cancer Center and Philadelphia Magazine

