Philly Has Higher Rates of Mortality Following Cardiac Arrest Than Other Large Cities. Activists Want to Change That.
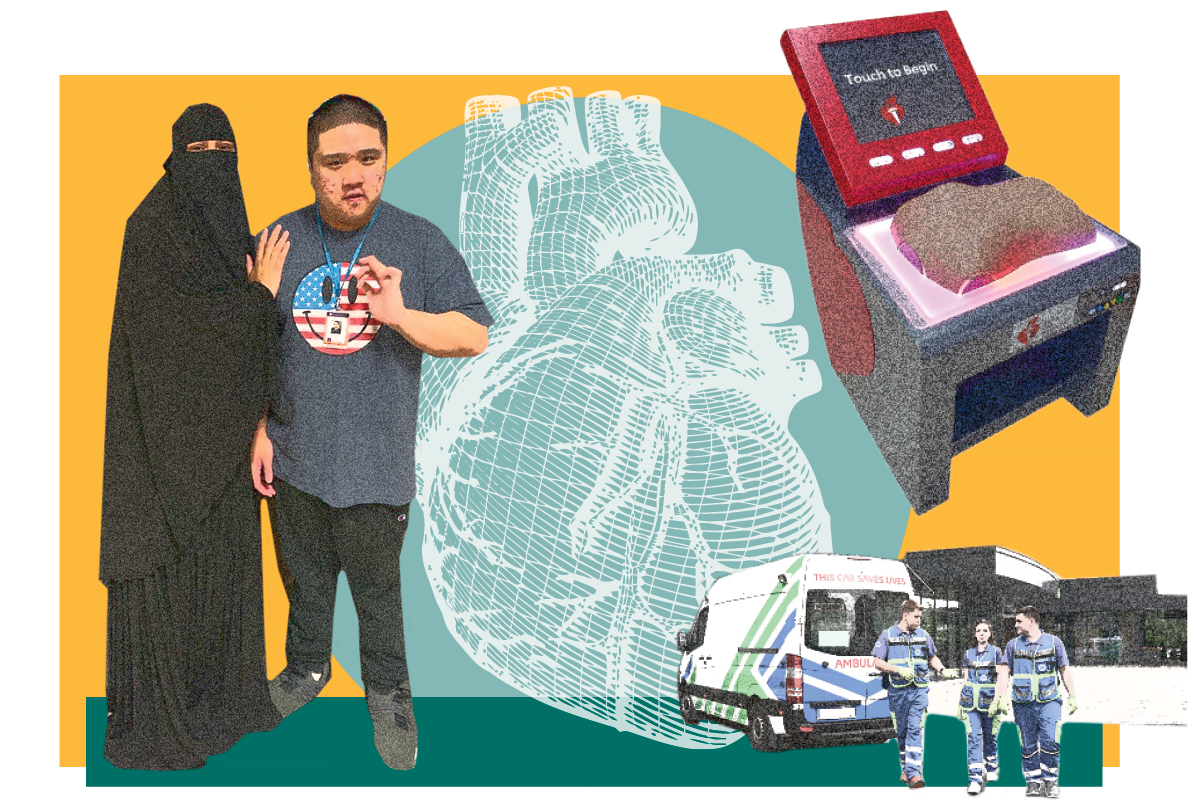
When a student yelled into the front office that a boy had collapsed in front of the school, Stephanie Williams, a school improvement support liaison at John Bartram High School, didn’t have time to doubt her training. As kids shuffled in for the beginning of the school day, she ran nonstop to the road, toward a huddle of adults and children. The boy, a student with a history of seizures, had fallen and hit his head. He wasn’t breathing, his skin was pale, and his lips were blue. As a former special needs assistant, Williams had been required to become certified in CPR. She had never had to use it before, but now she started doing chest compressions without a second thought.
“If you just apply the training that the instructor gave you,” Williams says, “you’ll remember everything that you were taught.” After several rounds of compressions, the boy gasped for air. By that time, the EMTs had arrived.
Brown was lauded as a hero by the school for her efforts. But Philadelphia hasn’t been able to depend on that kind of heroism for every case of cardiac arrest. According to Rich Snyder at Independence Blue Cross, Philadelphia has a higher rate of death following cardiac arrest than other cities of similar size that have focused on CPR education and AED use. When Snyder began looking into the problem in 2015, only 14 percent of people who experienced cardiac arrest outside of the hospital in Philadelphia received CPR. Other cities have programs designed to increase the number of people trained in CPR. Seattle and Phoenix, for instance, see more than 40 percent of their residents receive CPR outside the hospital.
“We know from experience that administering CPR immediately until help arrives increases survival rates materially,” Snyder says. As a board member of the American Heart Association, Snyder set about seeing how Philadelphia could get its rates closer to 40 percent. One measure was advocacy for a now-passed legal requirement in Pennsylvania to teach students CPR in school before graduation. Another has been the creation of mobile CPR training units to provide training in the neighborhoods that need it most. As Snyder notes, cardiac arrest and a failure to respond with CPR is a key driver of the fact that there can be a 20-year difference in lifespan between Philadelphia neighborhoods.
Those CPR-training efforts promise long-term results. One of the fastest solutions, however, has been the placement of CPR training kiosks in high-foot-traffic locations around the city. Training kiosks placed in the Independence Visitors Center and the Perelman Center at UPenn have trained more than 23,000 individuals in hands-only CPR, and Snyder says there are documented cases of lives being saved as a result of self-training at a kiosk.
A new mobile kiosk, which launched at the Wells Fargo Center in December, allows the American Heart Association to target more key gathering points. The mobile kiosk’s next stop will be Enon Tabernacle in Northwest Philadelphia. In a short time, the kiosks have shown a measurable impact.
“The combination of efforts, including the kiosks, neighborhood-and school-based training, took us from about 14 percent of patients outside of the hospital getting CPR when they had a cardiac arrest to 22 percent. And the survival rate in the city went from 20 percent to 26 percent between 2015 and 2020,” Snyder says.
In the meantime, Williams is focused on getting students at her school trained. Through a club at her school, she teaches students how they can save lives, just like she once did.
This is a paid partnership between Go Red For Women and Philadelphia Magazine