Philly Physicians Are Honing in on the Genetics of Common, Often-Deadly Lung Cancers–and Changing Survival Expectations

(l) Hossein Borghaei, DO, MS, Chief, Thoracic Medical Oncology, Fox Chase Cancer Center; (r) Julia Judd, DO, Assistant Professor, Department of Hematology/Oncology, Fox Chase Cancer Center
A lung cancer diagnosis can be particularly alarming, and it’s intuitive as to why—in addition to growing in the lungs, which enable breath and life, the cancer is rooted in the center of the body, making it easier to spread, and more difficult to remove. These factors act as dangerous drivers for the disease, and present oncologists and their patients with one of the toughest puzzles imaginable.
But contemporary cancer treatment, through innovative applications of our understanding of cancer cell genetics, is about reaching and destroying cancer where, previously, it might be otherwise difficult or impossible to do so, without damaging healthy tissue. And in the past few years, that revolutionary approach has started to transform our understanding of lung cancer’s difficult riddle.
Non-small cell lung cancer (NSCLC) is the most common type of lung cancer, and even when caught early, the risk of recurrence remains high. That means there are a lot of patients who can benefit from new advances in early-stage treatment–and in the past few years, innovative treatments that can help a wide spectrum of these patients.
“The data in the U.S. suggests that maybe about 30 percent and perhaps more of NSCLC patients in the U.S. could have an actionable mutation also called a biomarker such as EGFR,” says Dr. Hossein Borghaei, DO, MS, Chief, Thoracic Medical Oncology, Fox Chase Cancer Center, referring to a common driver of NSCLC. Treating that EGFR mutation, as well as other shifts in the way NSCLC is understood on a genetic level, have led to studies with pronounced results, up-ending survival rates established before the new treatments.
As a result, the use of immunotherapy or targeted therapy have rapidly become a critical part of care, enabling physicians to shrink the cancer, contain its spread, and occasionally make it possible to remove the cancer surgically, without pursuing treatment routes that may be harder on the patient’s health. And as physicians like Borghaei and Julia Judd, DO, Assistant Professor, Department of Hematology/Oncology, Fox Chase Cancer Center, continue to unlock these structures, they’re providing new hope to those for whom a diagnosis of lung cancer may have previously left them with little.
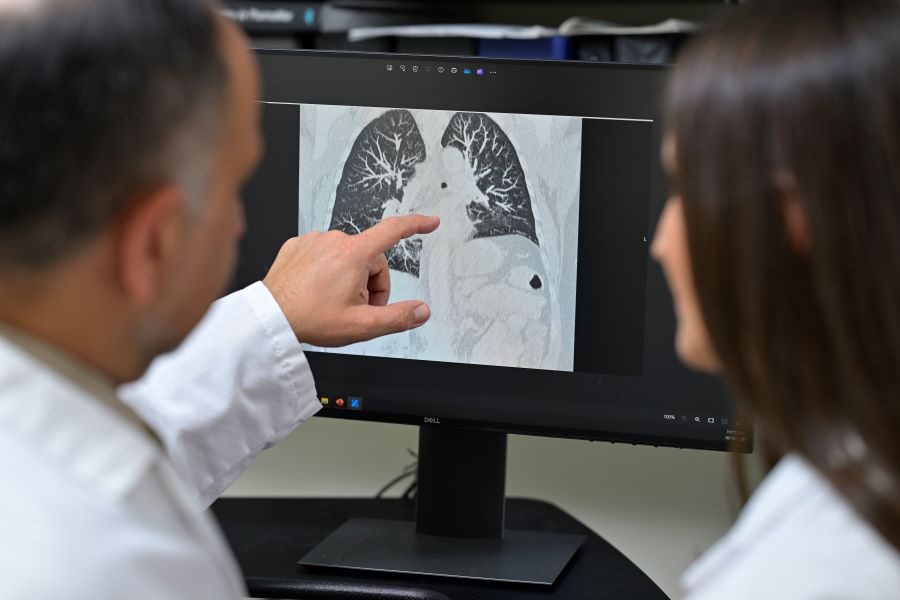
Examining a lung cancer scan.
The Start of a Solution
The revolution in NSCLC treatment can be traced to a deeper understanding of the disease at the molecular level. The new science of genetic testing, when applied to NSCLC, has uncovered mutations that drive cancer growth. Critically, this includes the commonly occurring EGFR mutations, which drives cancer growth by signaling to cells to continue multiplying.
Targeted therapies can tackle the EGFR mutations, without significantly affecting surrounding tissue, in contrast with traditional treatments like radiation and chemotherapy. Known as EGFR inhibitors, they block the mutation’s signal to slow or halt cancer progression. These include therapies such as Osimertinib, which “for up to about three years clearly showed a survival advantage in keeping the disease away when given after surgical resection,” Borghaei says.
Immunotherapies have similarly revolutionized NSCLC treatment by harnessing the body’s own defenses. NSCLC tumors often evade the immune system by exploiting a protein, known as PD-L1, that regulates the body’s immune response. Drugs like pembrolizumab and nivolumab block these checkpoints, allowing the immune system to recognize and attack tumor cells—demonstrated in a large study led by Borghaei which showed nivolumab improved long-term outcomes for patients with advanced NSCLC.
“The immunotherapy works by taking the brakes off the immune system and creating an immune response against the cancer,” says Judd. Immunotherapy also enables T-cells to better identify and attack even those cancer cells that have spread to distant areas, significantly reducing the risk of recurrence and improving long-term outcomes.

Examining a cancer biopsy.
Tackling Early-Stage Cancers
Since the positive effects of these therapies occur over time, they’re often thought of as a treatment used to prevent recurrence, and in NSCLC, they were initially applied primarily to combat metastatic cancer. But surprisingly, early-stage treatment with immunotherapy and targeted therapies has proven particularly effective for NSCLC.
“We learned from advances in metastatic settings that immunotherapy is effective,” Judd says, explaining that once they saw results in managing late-stage cancer, they began to pursue trials in treating early-stage disease, and they were surprised by just how effective the treatments were.
“We’re seeing immunotherapy create lasting immune responses, particularly when used in early-stage disease,” Borghaei says. Why would a drug be as effective, or even more effective, in an early stage versus a late stage? According to Borghaei, one reason may be that by the time a tumor becomes metastatic in stage IV, it has acquired additional mutations that make it more resistant to treatment, whereas early-stage lung cancer might not have developed those mutations.
In addition, a critical challenge in treating NSCLC is its tendency to spread early through micro-metastatic sites—small, undetectable clusters of cancer cells that are not visible through imaging. Even after successful surgery, these clusters can grow and lead to recurrence, making them a significant target in NSCLC treatment. Immunotherapy offers a powerful solution here, as it activates the body’s immune system to work systemically, hunting down and destroying cancer cells beyond the primary tumor.
“The neoadjuvant approach stimulates the immune system not just to attack the tumor but also to address any potential micro-metastatic disease,” Borghaei says. It’s possible that the earlier the patient receives the immunotherapy, the greater the impact the immunotherapy can have on these micro-metastatic sites.
Delivering Hope
Now, targeted therapies and immunotherapies are increasingly used before and after surgery to improve outcomes, and the results are changing NSCLC treatment from beginning to end. (Note: targeted therapy is not FDA-approved prior to surgery, only after.) For example, neoadjuvant chemotherapy combined with immunotherapy has shown promise in shrinking tumors, making surgery less invasive.
“Patients with fairly advanced disease, like stage 3, could benefit from chemo-immunotherapy. In fact, the benefit in that group might be even higher,” Borghaei says. “We are seeing some cases where surgery can be minimized to just a lobectomy.” For example, what would have required a pneumonectomy (removal of an entire lung), can now be treated with a lobectomy, preserving more lung function.
In other cases, these therapies can be used in place of chemotherapy, meaning they’re improving quality of life, with immunotherapy often causing fewer side effects than traditional chemotherapy. “The toxicity profile of immunotherapy is more manageable than chemotherapy,” Judd says.
“Moreover, the toxicity profile of neoadjuvant chemo-immunotherapy is manageable for most patients, and the addition of immunotherapy did not increase the incidence or severity of side effects,” Judd says.
Perhaps even more importantly, the impact of immunotherapy and targeted therapies on the success of NSCLC treatment has been profound. For the first time, physicians are seeing significant improvements in survival rates, particularly in early-stage disease. Multiple large, randomized trials have shown that combining chemotherapy and immunotherapy before surgery led to higher complete pathological response rates—meaning no viable tumor cells remained at surgery—compared to chemotherapy alone. “In one study a 22 percent improvement over chemotherapy alone was reported, which is clinically meaningful because more patients will live longer without their cancer recurring and are more likely to be cured,” Judd says.
Additionally, treatments like Osimertinib have revolutionized care for patients with EGFR mutations, offering hope for long-term survival. “Osimertinib was clearly shown to extend survival in the ADAURA trial,” Borghaei says. “It showed a 50 percent reduction in the risk of death at five years. That’s huge,” Judd adds.
The recency of these discoveries mean the field of NSCLC treatment is still evolving. Researchers are focused on discovering further biomarkers or refining biomarkers like PD-L1, which both Borghaei and Judd describe as imperfect, due to the difficulties in correctly determining its presence in the tumor. Ongoing research is also exploring the further use of combination therapies to have success without the presence of PD-L1, even patients with low levels of the protein present in their tumor can respond well to immunotherapy.
“We know that when chemotherapy is combined with a checkpoint inhibitor, it is active even in PD-L1-negative tumors,” Judd says. As our understanding of NSCLC’s molecular landscape deepens, the future promises even more personalized treatments tailored to each patient’s tumor biology. The revolution in lung cancer care is still unfolding, offering new hope.
“It’s rapidly evolving,” Judd says. “This was a very, very busy year in the world of lung cancer knowledge and therapy.”
This is a paid partnership between Fox Chase Cancer Center and Philadelphia Magazine
