Electricity Could Be a Transformative Prostate Cancer Treatment. These Philly Doctors Are Leading the Change
Sometimes the biggest innovations bring the right approach and technology together to create more than the sum of its parts. Right now, in Philadelphia, a revolutionary treatment is being studied, and the innovation is centered on something surprisingly commonplace–electricity.
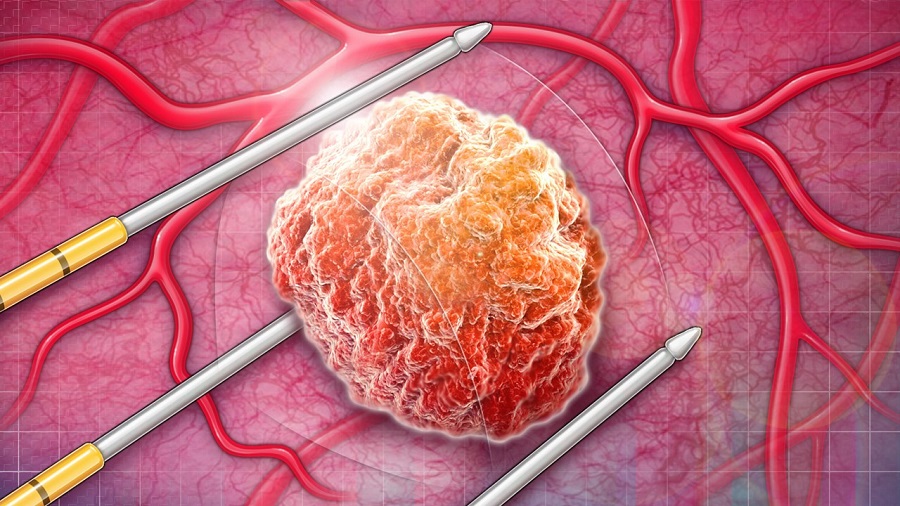
NanoKnife technology uses targeted electricity transmitted through two tiny rods to zap cancer cells in a hyper-specific spot in the body. That innovation, when brought to its full potential, carries huge implications, which are currently being explored at Fox Chase Cancer Center. They’re using the new technology in an innovative way to tackle an enduring challenge in prostate cancer, where treatment presents the risk of life-changing side effects, from sexual dysfunction to incontinence.
Using NanoKnife technology to try to avoid those side effects while eliminating cancer cells could prove transformative for not only prostate cancer–it could point to potential solutions for other cancers in sensitive areas where treatment carries the risk of side effects. Here’s how Philly physicians seek to make a major step forward in cancer care.
Finding a Third Option
The innovative use of NanoKnife technology is part of a new approach that runs counter to decades of a standard approach to prostate cancer.
A cancer diagnosis is always a psychological burden to face, but prostate cancer can also be scary because of the side effects of treatment. Traditional approaches to prostate cancer treatment have offered two primary options: low-risk prostate cancer is often left alone, with a ‘watchful waiting’ approach, while high-risk prostate cancer requires radiotherapy or surgical treatment of the entire prostate. That historical radical treatment, while often successful, carries the risk of side effects that can greatly affect the quality of life, including sexual dysfunction, incontinence, and bowel function changes.
While the safest course of action is often the correct course of action, many patients don’t fit cleanly into the high-risk versus low-risk binary when it comes to selecting a cancer treatment. For those patients, the standard default approach is often to treat the whole prostate aggressively anyway–-and that may not be a patient’s best option.
“Intermediate-risk disease is kind of this middle ground where we really don’t know if we’re overtreating or undertreating patients. It’s a very grey area,” says Dr. David Y. Chen, a urologic oncologist at Fox Chase. “We already know from large population studies that prostate cancer is probably overtreated. The odds are we’re probably treating many men who may not need or benefit from treatment.”
Dr. Andres F. Correa (left) and Dr. David Y. Chen (right) are working on revolutionizing prostate cancer treatment.
But in recent years, a new approach has begun to gain acceptance–and Chen and his colleague Dr. Andres F. Correa, a urologic oncologist at Fox Chase Cancer Center, are trying to bring that approach to more patients. New imaging capabilities have led to the increased use of focal therapy, a type of treatment in which physicians target cancers still localized within a certain prostate area and eliminate them with high confidence.
Chen compares this to breast cancer treatment. A total mastectomy was the primary solution for breast cancer treatment for many years. Once imaging advanced to the point where cancer could be identified earlier in smaller areas, localized surgery was used to spare the breast.
“The ability to see the equivalent, early small cancer in a prostate has become more of a possibility because of high-resolution MRI scans,” Chen says. “The idea of ‘let’s just treat that area as opposed to the entire prostate’ has really become more of a reality and less of just a concept.”
For patients with intermediate risk prostate cancer, this approach allows them to get a little bit of the best of both worlds.
“This is an intermediate step in the appropriately selected man, in which we’re not doing nothing, but we’re also not subjecting them to the same sort of radical treatment that we’ve historically felt was needed,” Chen says.
The Right Combination
Now, Chen and Correa are taking that approach and bringing it to its next stage through use of NanoKnife, which uses electricity to eliminate the targeted cancer cells while avoiding collateral damage and resultant side effects. In other words, they’re pairing the more exact imaging with a more exacting procedure.
“It allows you to direct the treatment and be a little bit less destructive around healthy tissues because your margin is a little bit tighter,” Correa says, explaining that a high voltage generated between the two probes effectively destroys the tissue. “So, when you’re hoping to spare either the urethra or a bundle of nerves, that technology is helpful now.”
Chen and Correa are working on making that approach the new standard.
“Technology only gets you somewhere, but most of it also comes from knowing what the technology can do and how far you can take it,” says Correa.
To that end, Dr. Correa and Dr. Chen are participating in a clinical trial at Fox Chase that is open nationally at multiple centers, involving NanoKnife technology. The Pivotal Study of the NanoKnife System for the Ablation of Prostate Tissue in an Intermediate-Risk Patient Population (PRESERVE) uses prostate-specific antigen tests, MRIs, and biopsies to monitor intermediate-risk patients following focal therapy and ensure they respond to NanoKnife treatment. If that trial is successful, it could lead to wider use of the approach.
“I’m hoping that in 10 to 15 years, I’m doing radical prostatectomy in a very limited number of patients,” Correa says. “To identify these [intermediate-risk] patients and marry that process with this treatment, I think, is going to be the future.”
This is a paid partnership between Fox Chase Cancer Center and Philadelphia Magazine

